Know about your eye conditions
Anophthalmia

ican (international children’s anophthalmia & Microphthalmia network) is a group for families and dedicated professionals taking part to lend support to those interested in learning more about anophthalmia and Microphthalmia.
You have just heard your baby has anophthalmia or microphthalmia (A/M). This is a difficult time. You may feel overwhelmed with grief and anger. You may instead be saying, the doctors must be wrong somehow. Or you may be rethinking every step of your pregnancy wondering what you did or did not do that could have caused this to happen. All of these are normal reactions to such unexpected news. YOU ARE NOT ALONE!
For Parents Support group Visit http://www.anophthalmia.org
ican Parents Support Forum
anophthalmia and Microphthalmia are rare conditions, and affect children worldwide. As such, most families will find themselves the only ones in their area coping with the stress of treating an anophthalmia or Microphthalmia child.
To help these families, ican has created an online support forum for families and friends worldwide to share their experiences with anophthalmia and Microphthalmia, their insight, and even success stories with others.
Please Note: This forum is heavily monitored for content abuse, and ican reserves the right to remove any posting that they feel doesn't conform to the purpose of the forum, and ban any member who posts questionable content.
Enter the ican Parents Support Forum
Anophthalmia is a medical term that is used to describe the absence of the globe and ocular (eye) tissue from the orbit. The terms Anophthalmia and Microphthalmia(A/M) (small eyes) are often used interchangeably since CT scans or MRI show some remnants of either the globe or surrounding tissue in most cases. Anophthalmia/Microphthalmia (A/M) may affect one eye with the other eye being normal, or both eyes, resulting in blindness.
A/M is rare, but the exact incidence is unknown. One report from a prospective study of 50,000 newborns found an incidence of microphthalmia of 0.22 per 1,000 live births. In a recent study in England, the prevalence of anophthalmia and microphthalmia was 1.0 per 10,000 births.
A/M can be congenital (present at birth) or acquired later in life. A/M can occur alone or along with other birth defects. A/M may result from inherited genetic mutations, sporadic genetic mutations, chromosome abnormalities, prenatal environmental insult or other unknown factors.
Prevalence
True or primary anophthalmos is very rare. Only when there is complete absence of the ocular tissue within the orbit can the diagnosis of true anophthalmos be made. Extreme microphthalmos is seen more commonly. In this condition, a very small globe is present within the orbital soft tissue, which is not visible on initial examination.
There are three classifications for this condition:
- Primary anophthalmia is a complete absence of eye tissue due to a failure of the part of the brain that forms the eye.
- Secondary anophthalmia the eye starts to develop and for some reason stops, leaving the infant with only residual eye tissue or extremely small eyes which can only be seen under close examination.
- Degenerative anophthalmia the eye started to form and, for some reason, degenerated. One reason for this occurring could be a lack of blood supply to the eye.
Anophthalmia and microphthalmia may occur secondary to the arrest of development of the eye at various stages of growth of the optic vesicle. It is important to recognize microphthalmia because the development of the orbital region, as well as the lids and fornices, is dependent upon the presence of a normal-sized eye in utero. Anophthalmia is sometimes a clinical characteristic of Trisomy 13 (Patau syndrome) which is a Gross Chromosomal Abnormality.
TYPES: Consecutive anophthalmia, primary anophthalmia, and secondary anophthalmia.
Early treatment with various expanders or surgery, when necessary, will help decrease the orbital asymmetry and cosmetic deformities in these children.
Microphthalmia


Resources for the Blind or Visually Impaired
GeneReviews: Anophthalmia/Microphthalmia Overview
www.geneclinics.org
American Society of Ocularists
www.ocularist.org
American Foundation for the Blind
www.afb.org
National Association for Parents of Children with Visual Impairments
www.spedex.com/napvi
Micro and Anophthalmic Childrens Society
www.macs.org.uk
Welcome to Blind Links
http://seidata.com/~marriage/rblind.html
National Federation of the Blind
www.nfb.org
American Printing House for the Blind
www.aph.org
Social Security Administration,
If you are Blind or Have Low Vision – How we Can Help
www.ssa.gov/pubs/10052.html
American Society of Opthalmic Plastic and Reconstructive Surgery
www.asoprs.org
National Society of Genetic Counselors
www.NSGC.org
American College of Medical Genetics
www.ACMG.net
Lions Club International
www.lionsclub.org
Microphthalmia Yahoo group
Microphthalmia (microphthalmos) is a congenital condition in which the eye(s) started to form during pregnancy but for some reason stopped, leaving the infant with small eye(s). The size of the eye can vary from child to child. If very mild, it can almost go unnoticed, but usually it is fairly obvious. At the other end of the scale there is extreme microphthalmia, which is almost the same as anophthalmia.
Complex Microphthalmos denotes an eye that is small and that has been found to have additional eye findings. These include cataract (clouding of the lens), coloboma(absence of a portion of a structure of the eye such as the iris, retina, and/or optic nerve), and orbital cyst. The degree of vision is dependent on the extent and location of the associated eye findings.
Microphthalmia, anophthalmia and coloboma are on a spectrum of eye abnormalities often referred to as MAC.
Presentation
The presence of a small eye within the orbit can be a normal incidental finding but in most cases it is abnormal and results in blindness. The incidence is 14 per 100,000 and the condition affects 3-11% of blind children.
[edit]Causes
The major causes for this disorder are genetic but environmental factors have also been implicated such as exposure to radiation, chemicals, or viruses. Microphthalmia in newborns is sometimes associated with fetal alcohol syndrome[1] or infections during pregnancy, particularly herpes simplex virus, rubella and cytomegalovirus (CMV), but the evidence is inconclusive. Genetic causes of microphthalmia include chromosomal abnormalities (trisomy 13 (Patau syndrome), Triploid Syndrome, and Wolf-Hirschhorn Syndrome) or monogenetic Mendelian disorders. The latter maybe autosomal dominant, autosomal recessive or X linked. Genes that have been implicated in microphthamia include many transcription and regulatory factors. Those identified from family studies include the following:
| HGNC symbol | Description | OMIM | Type |
|---|---|---|---|
| BCOR | BCL6 corepressor | 300166 | MCOPS2 |
| CRYBA4 | crystallin, beta A4 | ||
| FOXE3 | forkhead box E3 | ||
| GDF6 | growth differentiation factor 6 | ||
| MITF | microphthalmia-associated transcription factor | ||
| OTX2 | orthodenticle homeobox 2 | ||
| PAX6 | paired box 6 | ||
| PITX3 | Paired-like homeodomain transcription factor 3 | ||
| RAX | retina and anterior neural fold homeobox | ||
| SHH | sonic hedgehog homolog | ||
| SIX6 | SIX homeobox 6 | ||
| SOX2 | SRY (sex determining region Y)-box 2 | 206900 | MCOPS3 |
| VSX1 | visual system homeobox 1 | ||
| VSX2 (CHX10) | visual system homeobox 2 |
Development of the eye during pregnancy is a very complex process. Many genes are involved in ensuring that the sequence of this development occurs as it should. The eye is completely developed in the first trimester of pregnancy.
There are many known causes of anophthalmia, microphthalmia and coloboma including genetic conditions and prenatal exposures to infections and medicines. However, in most cases the cause is unclear.
Genetic research
Researchers around the world are working to identify the genes involved in the normal development of the eye. Many genes have been found to have a role in this complicated process. Changes in these genes, also known as mutations, can cause the gene to not work properly causing abnormal development of the eye.
Most changes (mutations) in a gene have occurred for the first time in the individuals with anophthalmia/microphthamia. In other words there is no family history of the condition. This does not mean the cause is not genetic.
Identifying the cause of the eye defect is important in terms of management of the individual medically and educationally. In addition, risks for recurrence differ based on the reason that the eye defect occurred.
What is SOX2 syndrome?
People with SOX2 syndrome are usually born with anophthalmia, although some individuals have microphthalmia. The anophthalmia or microphthalmia can be in one eye or both.
Individuals with SOX2 syndrome may also have seizures, brain abnormalities, slow growth, delayed development of motor skills (such as walking), and mild to severe learning disabilities. Some people with this condition are born with a blocked esophagus (esophageal atresia), which is often accompanied by an abnormal connection between the esophagus and the trachea (tracheoesophageal fistula). Genital abnormalities have been described in affected individuals, especially males.
How common is SOX2 syndrome?
SOX2 syndrome is estimated to affect 1 in 250,000 individuals. About 10 percent to 15 percent of people with anophthalmia in both eyes have SOX2 syndrome.
How do people inherit SOX2 syndrome?
Mutations in the SOX2 gene cause SOX2 syndrome and is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. Most cases result from new mutations in the SOX2 gene. This means there is no history of the disorder in their family. In a small number of cases, people withSOX2 syndrome have inherited the changed gene from an unaffected parent who has aSOX2 mutation only in their sperm or egg cells. This phenomenon is called germline mosaicism.
This gene was identified several years ago by researchers in England. Changes (mutations) in this gene have been found in about 15% of individuals with anophthalmia/microphthalmia. Typically an individuals has 2 working copies of this gene. If one copy is changed (mutated) it leads to anophthalmia/microphthalmia. Genetic testing is available for SOX2 and should be ordered on anyone with anophthalmia or microphthalmia. If you need help getting this test done call Tanya Bardakjian 215-456-8726 or e-mail bardakjiant@einstein.edu.
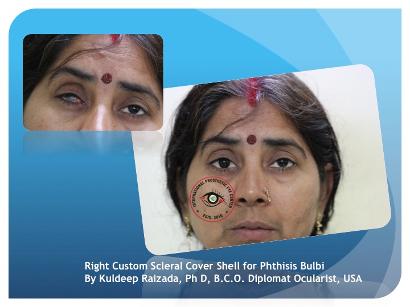
Phthisis bulbi

| |
| |
| |
| |
| |
| |
|
Evisceration of eye
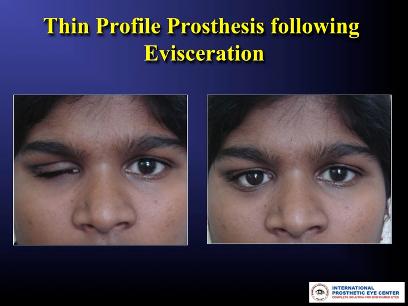
An evisceration is the removal of the eye's contents, leaving the scleral shell and extraocular muscles intact.[1][2] The procedure is usually performed to reduce pain or improve cosmesis in a blind eye, as in cases of endophthalmitis unresponsive to antibiotics.[1][2] An ocular prosthetic can be fitted over the eviscerated eye in order to improve cosmesis.[3]
Either general or local anesthetics may be used during eviscerations, with antibiotics and anti-inflammatory agents injected intravenously.
Know about Bio Eye
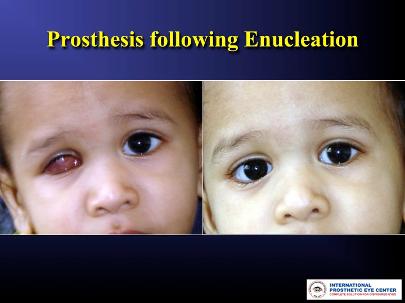
Enucleation of the eye
Retinoblastoma International is dedicated to eliminating the devastating effects of children’s eye cancer and its complications worldwide.
Download more information about Retinoblastoma International
Know the Glow: for General Public awareness and General Physicians
Enucleation is removal of the eye, leaving the eye muscles and remaining orbital contents intact. This type of ocular surgery is indicated for a number of different ocular tumors, in eyes that have suffered severe trauma, and in eyes that are blind and painful owing to other disease.[1]
Auto-enucleation (oedipism) and other forms of serious self inflicted eye injury are an extremely rare form of severe self-harm which usually results from serious mental illnesses such as schizophrenia.[2] The name comes from Oedipus, who gouged out his eyes in penance after having sex with his mother and killing his father.[3] Some patients have apparently been inspired by the Gospel of Matthew, which states: "...if the right eye offend thee, pluck it out and cast it from thee" (5:29).[4]
Classification
There are three types of eye removal
- Evisceration - removal of the internal eye contents, but the sclera is left behind with the extraocular muscles still attached.
- Enucleation - removal of the eyeball, but the adjacent structures of the eye socket and eyelids remain. An intraocular tumor excision requires an enucleation, not an evisceration.
- Exenteration - removal of the contents of the eye socket (orbit) including the eyeball, fat, muscles and other adjacent structures of the eye. The eyelids may also be removed in cases of cutaneous cancers and unrelenting infection. Exenteration is sometimes done together with Maxillectomy which is removal of the maxilla or the upper jaw bone/cheekbone
Reasons for eye removal
- Cancer of the eye (retinoblastoma, melanomas, any other cancers of the eye or orbit)
- Severe injury of the eye when the eye cannot be saved or attempts to save the eye have failed
- End stage glaucoma
- Painful, blind eye
- In cases of sympathetic ophthalmia (inflammation of the eye) to prevent travel to other eye, in which, if untreated can cause blindness
- Congenital cystic eye
- In a deceased person, so the cornea can be used for a living person who needs a corneal transplant by a surgical operation called keratoplasty.
- Constant infection in a blind, or otherwise useless eye.
Orbital implants and ocular prostheses
Removal of the eye by enucleation or evisceration can relieve pain and minimize further risk to life and well-being of an individual with the above noted conditions. In addition, procedures to remove the eye should address the resultant appearance of the orbit. Orbital implants and ocular prostheses are used by the surgeon to restore a more natural appearance.
An orbital implant is placed after removal of the eye to restore volume to the eye socket and enhance movement or motility of an ocular prosthesis and eyelids. The eyeball is a slightly elongated sphere with a diameter of approximately 24 millimetres. To avoid a sunken appearance to the eye socket, an implant approximating this volume can be placed into the space of the removed eye, secured, and covered with Tenon's capsule and conjunctiva (the mucous membrane covering the natural sclera). Implants can be made of many materials with the most common being plastic,hydroxylapatite, metal alloy or glass.
Later, once the conjunctiva have healed and post-operative swelling has subsided, an ocular prosthesis can be placed to provide the appearance of a natural eye. The prosthesis is fabricated by an ocularist. Its form is that of a cupped disc so that it can fit comfortably in the pocket behind the eyelids overlying the conjunctiva that covers the orbital implant. The external portion of the ocular prosthesis is painted and finished to mimic a natural eye color, shape and luster. It can be removed and cleaned periodically by the individual or a care giver.
The two part system of orbital implant and ocular prosthesis provides a stable, and well tolerated aesthetic restoration of the eye socket. Although vision is not restored by removal of the eye with placement of an orbital implant and ocular prosthesis, a natural appearance can result. The implant can be moved by intact extraocular muscles that will track or move simultaneously with the other eye. The visible ocular prosthesis can couple with the orbital implant and thus move simultaneously with the other eye. The eyelids can move and blink over the prosthesis as well.
Prosthetic eye to treat blindness: at an early
Sheila Nirenberg:
A prosthetic eye to treat blindness
Uploaded on Dec 20, 2011
http://www.ted.com At TEDMED, Sheila Nirenberg shows a bold way to create sight in people with certain kinds of blindness: by hooking into the optic nerve and sending signals from a camera direct to the brain.
TEDTalks is a daily video podcast of the best talks and performances from the TED Conference, where the world's leading thinkers and doers give the talk of their lives in 18 minutes. Featured speakers have included Al Gore on climate change, Philippe Starck on design, Jill Bolte Taylor on observing her own stroke, Nicholas Negroponte on One Laptop per Child, Jane Goodall on chimpanzees, Bill Gates on malaria and mosquitoes, Pattie Maes on the "Sixth Sense" wearable tech, and "Lost" producer JJ Abrams on the allure of mystery. TED stands for Technology, Entertainment, Design, and TEDTalks cover these topics as well as science, business, development and the arts. Closed captions and translated subtitles in a variety of languages are now available on